50 yrs old male k/c/o HbsAg +ve with cirrhosis
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Team:
Interns-
M Supriya
Mohitha
K Sowmya
Sanjay
Amrutha
Dr.Druga Krishna PGY1
Dr.Ajith Kumar PGY2
Dr.Laxma Reddy PGY3
Dr.Manasa PGY3
Dr.Vijaya Lakshmi (Ast.Prof.)
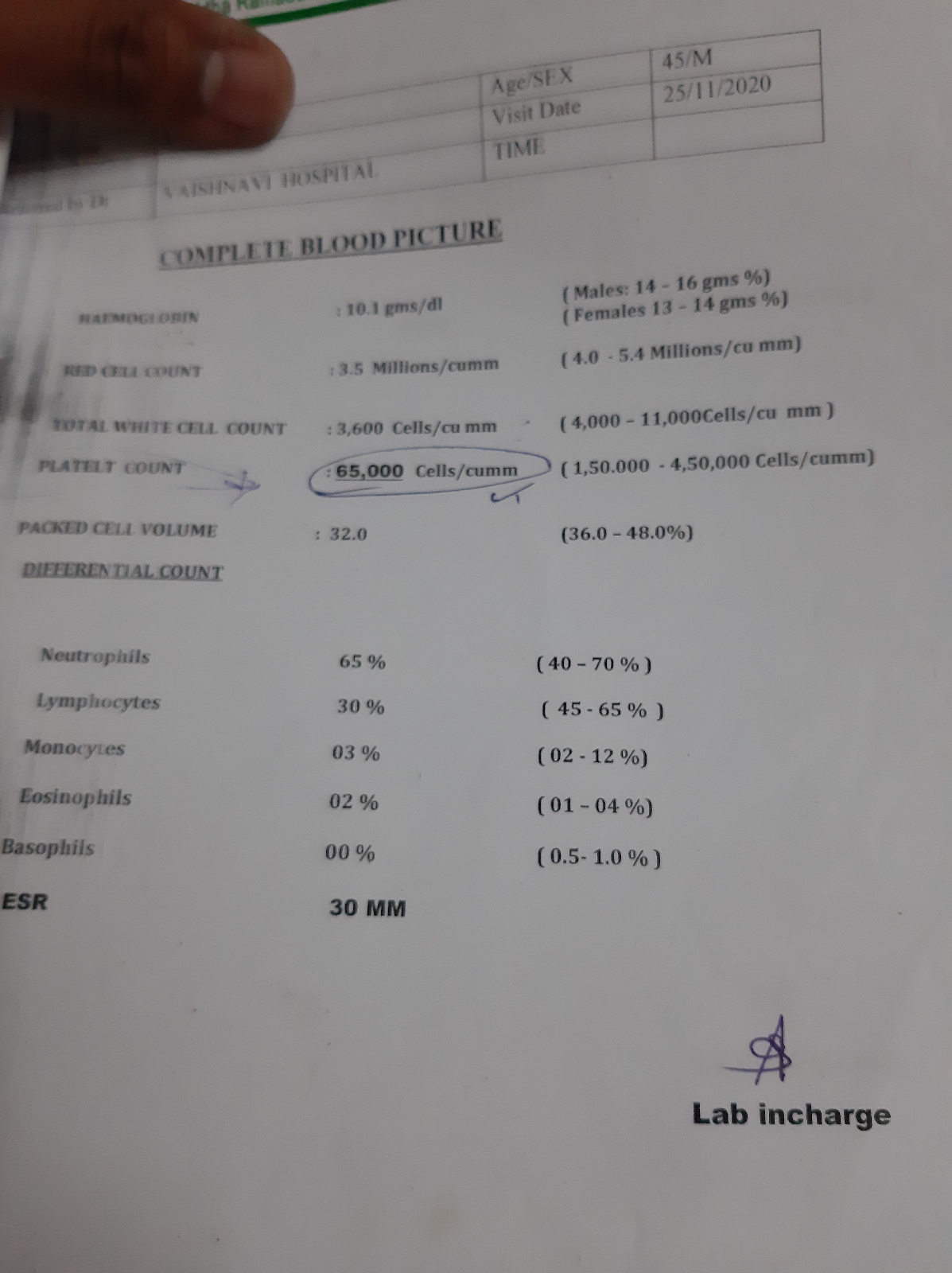
pt was apparently asymptomatic 7 months back then he developed low grade fever with yellowish discolouration of eyes followed by pedal edema which is gradually progressive and pitting type -no aggrevating and relieving factors,then he developed abdomenal distenstion which was insidious onset and gradually progressive along with H/o decreased urine output then pt went to the local Hospital and started on conservative management then pt symptoms were relieved then pt had repeated follow up to the local Hospital..in the month of November pt was diagnosed with Hbsag+ve ..and no where ascitic tap was done or attempted .previous report form november showed his platelet count was 65,000
Hb 11.2%. pt had on and off symptoms ...His aggravating factors are Non veg food ,taking toddy ..and Relieving factors are Vegeterian diet and Medication usage.
past history
previous reports
k/c/o HbsAg since 3month
Not a k/c/o DM ,HTN,TB,Asthma ,epilepsy
personal history
personal history
Addictions- alcoholic since 20 yrs of age takes 90ml daily along with1 glass saara occasionally
pt had h/o death of his wife 3 yrs back from then his alcohol intake was increased from quarter to Half and toddy intake was also increased
O/E
Patient is conscious coherent coperative
Vitals
Bp -110/70
PR -87bpm
RR - 22 cpm
Spo2 98@room air
Systemic examination
Cvs -s1s2 +
Rs -BAE +
P/A -
-inspection-
Patient is conscious coherent coperative
moderately built
No signs of Icterus, cynosis, clubbing, lymphedenopathy, kilonycia
Vitals
Bp -110/70
PR -87bpm
RR - 22 cpm
Spo2 98@room air
Systemic examination
Cvs -s1s2 +
Rs -BAE +
P/A -
-inspection-
shape -distented ,
umbalicus-central and partially everted ,
stirae present above the umbilicus,
abdominal movements present on respiration,
no pulsatation,
engorged veins are present
-palpations-
no local rises of temperature,non tender,soft , non tender ,no organomegaly,
hernial orifices normal,
-percussion-
dull node on percussion is felt in epigastric region and flanks
shift in dullness present
fluid thrill present
-Auscultation-
Bowel sounds +
CNS -normal
Investigations
Treatment-
on the day of admission
1TAB SPIRONOLACTONE 50 MG/OD
2.TAB LASIX 40 MG/PO/TID
DAY 1
1TAB SPIRONOLACTONE 50 MG/OD
2.TAB LASIX 40 MG/PO/TID
DAY 2
1TAB SPIRONOLACTONE 50 MG/OD
2.TAB LASIX 40 MG/PO/TID
3.INJ VIT K 10 MG/IV/STAT
Provisional diagnosis-
k/c/o HbSAg +ve with cirrhosis